🔗 Mitochondrial dysfunction in acute and post-acute phases of COVID-19 and risk of non-communicable diseases https://www.nature.com/articles/s44324-024-00038-x
> Up to 70% of people affected by COVID-19 show reduced organ function even four months or more after COVID-19 diagnosis
> a comparative study of patients suffering from long COVID, and patients fully recovered from COVID-19, demonstrated a metabolic phenotype with dysfunctional mitochondria-dependent lipid catabolism for both groups, when compared to persons with no history of COVID-19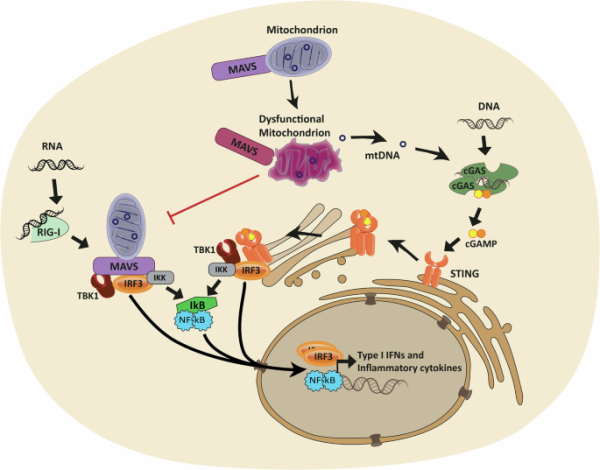
> Up to 70% of people affected by COVID-19 show reduced organ function even four months or more after COVID-19 diagnosis
> a comparative study of patients suffering from long COVID, and patients fully recovered from COVID-19, demonstrated a metabolic phenotype with dysfunctional mitochondria-dependent lipid catabolism for both groups, when compared to persons with no history of COVID-19
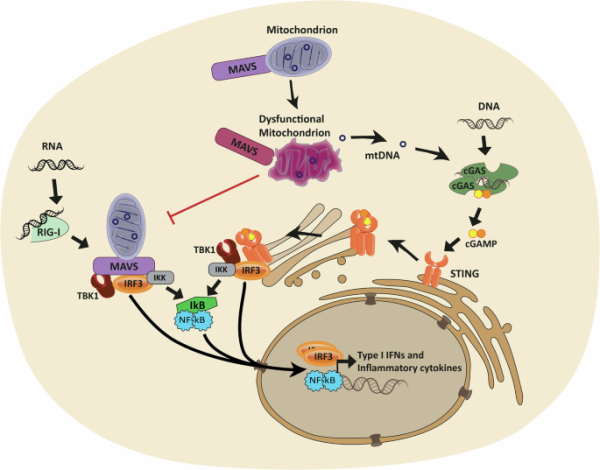
Mitochondrial dysfunction in acute and post-acute phases of COVID-19 and risk of non-communicable diseases - npj Metabolic Health and Disease
npj Metabolic Health and Disease - Mitochondrial dysfunction in acute and post-acute phases of COVID-19 and risk of non-communicable diseasesNature

trendless •
🔗 https://www.nature.com/articles/s44324-024-00038-x
Mitochondrial dysfunction in acute and post-acute phases of COVID-19 and risk of non-communicable diseases - npj Metabolic Health and Disease
Naturetrendless •
datum (n=1) •
In other words it would be a LESS FIT virus if it did NOT cause LC. Water runs downhill; viruses do not evolve to become less fit.
#LongCOVID #COVID #COVID19 #CovidIsNotOver
@trendless
Hugs4friends ♾🇺🇦 🇵🇸😷 hat dies geteilt