Suche
Beiträge, die mit chronicfatiguesyndrome getaggt sind
"Almost no ME/CFS patients return to work: "The help we have provided to patients through the welfare and healthcare systems has had little rehabilitative effect," says a researcher."
https://www.sciencenorway.no/chronic-fatigue-syndrome-diseases-me/almost-no-me/cfs-patients-return-to-work/2482762
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
1/
Study reveals that ME/CFS patients struggle to return to work
'The help we have provided to patients through the welfare and healthcare systems has had little rehabilitative effect,' says a researcher.Emilie Wee (ScienceNorway)
- Dr David Joffe: an overview of biological basis of Long COVID
- Dr David Tuller: on basis of psycho-behavioural therapy focusing on the PACE trial & a major #LongCOVID trial"
https://youtu.be/V9f_kjlz6Ho
From latest Science for ME update
@longcovid
#PASC #PwLC #postcovid #postcovid19 #LC #PostCovidSyndrome #COVIDBrain #NeuroPASC
@covid19 #Coronavirus
#SARSCoV2 #CovidIsNotOver
@auscovid19 #auscovid19
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
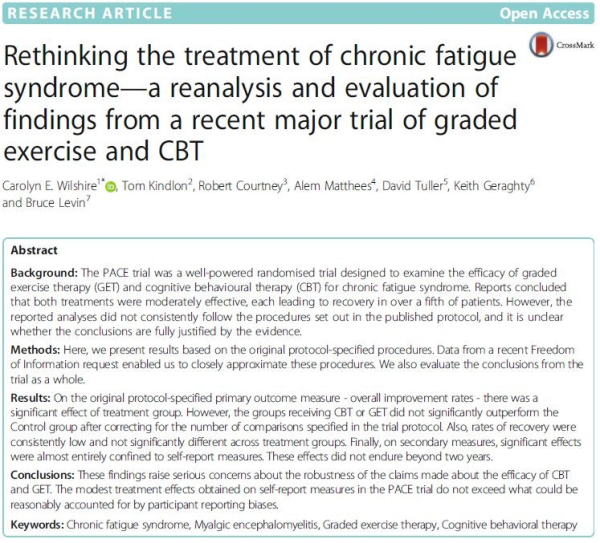
A lot of it was only possible due to Alem's heroic FOI victory, which the #PACETrial team fought so hard to stop.That surely wasn't because the real results weren't as flattering as they had presented them?
https://bmcpsychology.biomedcentral.com/articles/10.1186/s40359-018-0218-3
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Rethinking the treatment of chronic fatigue syndrome—a reanalysis and evaluation of findings from a recent major trial of graded exercise and CBT - BMC Psychology
Background The PACE trial was a well-powered randomised trial designed to examine the efficacy of graded exercise therapy (GET) and cognitive behavioural therapy (CBT) for chronic fatigue syndrome.BioMed Central
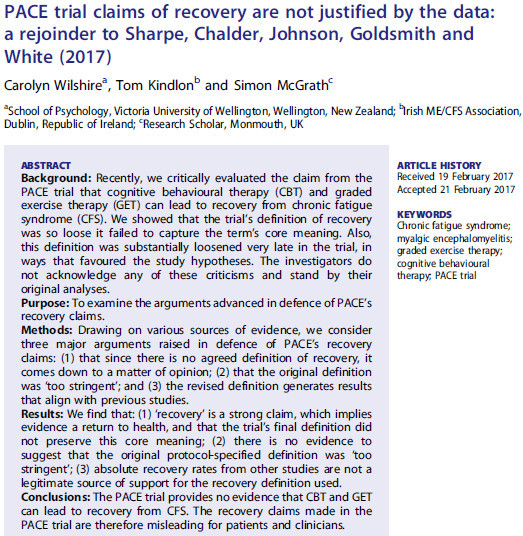
Free: https://researchgate.net/publication/315482747_PACE_trial_claims_of_recovery_are_not_justified_by_the_data_A_Rejoinder_to_Sharpe_Chalder_Johnson_Goldsmith_and_White_2017
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
https://www.jmir.org/2025/1/e59217/
From the latest Science for ME weekly update
@longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers #COVIDBrain #NeuroPASC
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME #POTS @pots
Opportunities and Challenges in Using Electronic Health Record Systems to Study Postacute Sequelae of SARS-CoV-2 Infection: Insights From the NIH RECOVER Initiative
The benefits and challenges of electronic health records (EHRs) as data sources for clinical and epidemiologic research have been well described.Journal of Medical Internet Research
https://appgme.co.uk/wp-content/uploads/2025/03/2025-03-05-APPG-on-ME-Minutes.pdf
From the latest Science for ME weekly update
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
https://www.emerge.org.au/researchdigest/research-digest-issue-114/
Includes new "Easy Read Overview" plus the option to hear the text
Hashtags:
@longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers #COVIDBrain #NeuroPASC
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Unusual but sympathetic paper:
Language Matters: What Not to Say to Patients with Long COVID, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, and Other Complex Chronic Disorders
https://www.mdpi.com/1660-4601/22/2/275
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME @longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers #COVIDBrain #NeuroPASC
1/
Language Matters: What Not to Say to Patients with Long COVID, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, and Other Complex Chronic Disorders
People with Long COVID, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), and other complex chronic disorders consistently report having difficulty obtaining effective and compassionate medical care and being disbelieved, judged, gaslighte…MDPI
Daily Drop about Long Covid ME/CFS updates: https://turnto.ai/download
#Covid
#LongCovid
#MECFS
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome
https://www.mdpi.com/1660-4601/22/2/280
"White respondents had 2.94 greater odds of being diagnosed with ME/CFS than non-White respondents"
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
https://research.manchester.ac.uk/en/studentTheses/what-is-the-psychological-and-educational-impact-of-being-an-emer
Screenshot from latest Science for ME weekly update
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Good Practice Guidelines for Psychologists Working with People with ME/CFS November 2024 Update
https://meassociation.org.uk/wp-content/uploads/2024/11/BPS-MECFS-Guidelines-Update-11.11.24.pdf
Although this isn't brand new, I found it interesting so I'm going to post some extracts to this thread.
#MEcfs #CFS #PwME @mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome
1/
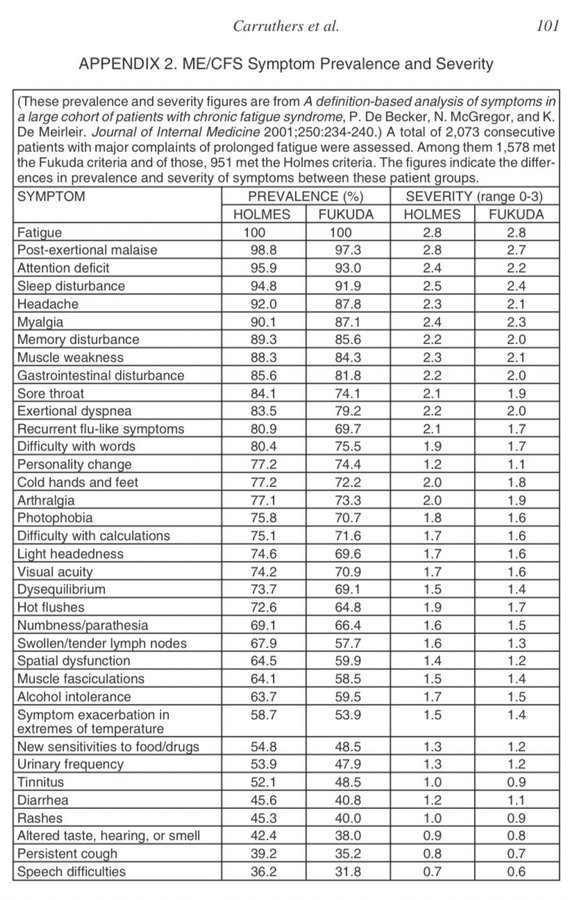
Particularly relevant when similarities with the #LongCovid presentation in some people are being missed
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
@longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers #COVIDBrain #NeuroPASC
https://investinme.org/iimer-newslet-cofefore24.shtml
@invest_in_me_research @mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Invest in ME Research - Centre of Excellence for ME Norwich Research Park
Invest in ME Research ICentre of Excellence for ME Norwich Research Parkinvestinme.org
Free:
https://pmc.ncbi.nlm.nih.gov/articles/PMC11537498/
Image is from free AMMES February 2025 e-newsletter
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
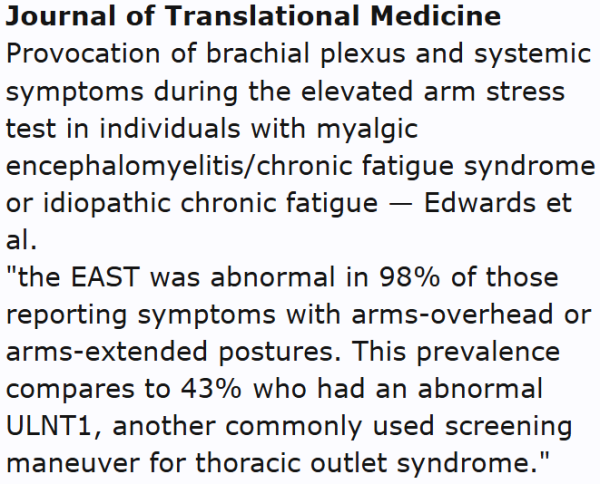
Provocation of brachial plexus and systemic symptoms during the elevated arm stress test in individuals with myalgic encephalomyelitis/chronic fatigue syndrome or idiopathic chronic fatigue
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06137-7
Image from latest Science for ME update
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Provocation of brachial plexus and systemic symptoms during the elevated arm stress test in individuals with myalgic encephalomyelitis/chronic fatigue syndrome or idiopathic chronic fatigue - Journal of Translational Medicine
Background We have noted that some adolescents and young adults with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) report difficulty with arms-overhead activities, suggestive of brachial plexus dysfunction or thoracic outlet syndrome (T…BioMed Central
[OI = orthostatic intolerance]
https://www.mdpi.com/2218-273X/15/1/102
Image is from the Science for ME latest update
#MEcfs #CFS #PwME
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome
Tetrahydrobiopterin in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Friend or Foe?
Myalgic Encephalomyelitis or Chronic Fatigue Syndrome (ME/CFS) is a chronic multisystem disease characterized by severe muscle fatigue, pain, dizziness, and brain fog.MDPI
https://www.nature.com/articles/s41598-025-85217-6
"The results of the MR analysis revealed no causal relationship between MDD & ME/CFS"
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
Relationship between major depressive disorder and myalgic encephalomyelitis/chronic fatigue syndrome: a two-sample mendelian randomization study analysis - Scientific Reports
Scientific Reports - Relationship between major depressive disorder and myalgic encephalomyelitis/chronic fatigue syndrome: a two-sample mendelian randomization study analysisNature
YouTube link:
https://www.youtube.com/watch?v=nskeLpbVMHg
It would be great if more people could subscribe to our channel
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME #LongCovid @longcovid
- YouTube
Auf YouTube findest du die angesagtesten Videos und Tracks. Außerdem kannst du eigene Inhalte hochladen und mit Freunden oder gleich der ganzen Welt teilen.www.youtube.com
“It’s a moving target”: Experiences of pacing to reduce symptom exacerbation among adults living with
#LongCOVID...an international community-engaged qualitative research study
https://www.medrxiv.org/content/10.1101/2024.12.11.24318864v1
Also relevant to #MECFS
@longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME
“It’s a moving target”: Experiences of pacing to reduce symptom exacerbation among adults living with Long COVID – Results from an international community-engaged qualitative research study
Introduction Long COVID is a multisystem condition that negatively impacts daily function. Pacing is a self-management strategy to mitigate symptoms.medRxiv
Immune T cells become exhausted in chronic fatigue syndrome patients
https://www.eurekalert.org/news-releases/1066876
Longer piece from same university with more quotes:
https://news.cornell.edu/stories/2024/12/immune-t-cells-become-exhausted-chronic-fatigue-syndrome-patients
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME @mecfs
Immune T cells become exhausted in chronic fatigue syndrome patients | Cornell Chronicle
The study found that key CD8+ T cells showed signs of constant stimulation that lead to an exhausted state, a condition that is well-studied in cancer.Cornell Chronicle
A lot of it focuses on ME/CFS, controversies but also tragedies such as people dying from the illness
https://www.scottishlegal.com/articles/david-j-black-economic-fallacies-and-public-health-realities
Includes mentions of Simon Wessely & #PACEgate
#MEcfs #CFS #PwME @mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome @disability
@disabilityjustice
David J Black: Economic fallacies and public health realities
In part two of his series on dysfunction in our health system, David J Black reminds us that the cost of bad medicine is people's lives. Read part one here.Scottish Legal News
"Despite broad criticism, the National Board of Health and Welfare will not update its knowledge support on post-infectious conditions."
Google English translation:
https://fof-se.translate.goog/artikel/socialstyrelsen-underkanner-whos-kunskapsunderlag-om-postcovid/?_x_tr_sl=auto&_x_tr_tl=en&_x_tr_hl=en-US&_x_tr_pto=wapp
Screenshot from Science for ME update
@longcovid
#LongCovid #PASC #PwLC #postcovid #postcovid19 #LC #Covidlonghaulers #PostCovidSyndrome #longhaulers
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME #POTS
Socialstyrelsen underkänner WHO:s kunskapsunderlag om postcovid
Socialstyrelsens kunskapsstöd om postinfektiösa tillstånd presenterades i augusti i år och fick då skarp kritik från läkare, forskare och patientföreningar – vilka ansåg att det …jonas.mattsson@fof.se (Forskning & Framsteg)
In it Dr David Systrom talks about new research on neurovascular issues in #MECFS & #LongCOVID
https://www.youtube.com/watch?v=TD-eSXKvfq
#PEM @mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME @longcovid
#LongCovid #PwLC #PostCovidSyndrome #LC #PASC #postcovid
- YouTube
Auf YouTube findest du die angesagtesten Videos und Tracks. Außerdem kannst du eigene Inhalte hochladen und mit Freunden oder gleich der ganzen Welt teilen.www.youtube.com
Thanks very much to David for his kind words on me in this. I have largely retired from writing papers, letters & e-letters and am very grateful to him for his ongoing work which takes a lot of ongoing commitment, plus dealing with many frustrating scenarios.
https://virology.ws/2024/11/13/trial-by-error-my-tour-of-ireland-through-wind-and-rain-slides-of-my-talk/
@mecfs
#MyalgicEncephalomyelitis #ChronicFatigueSyndrome #MEcfs #CFS #PwME @longcovid
#LongCovid #PASC #PwLC
1/
Trial By Error: My Tour of Ireland, Through Wind and Rain; Slides of My Talk | Virology Blog
By David Tuller, DrPH Last month, I took a quick speaking tour around Ireland at the invitation of the Irish ME/CFS Association. I first became acquainted w ...David Tuller (Virology Blog)